After 1980: Changing Trends in Hypertension Therapy
The VA and Framingham studies, public awareness campaigns, and the development of new hypertension drugs had begun changing medical and public attitudes about high blood pressure by 1980. However, it is one thing to know that treatment works, and quite another to integrate it into medical practice. Freis was moving forward with his clinical investigations, but as a leading expert in the field he also participated in ongoing discussions and debates about hypertension treatment. One focus of discussion was whether and when to treat "borderline" high blood pressure. Should a decision be based on blood pressure measurement alone? What other factors should be considered? And should initial treatment always include medication? Freis devised a scoring system based on risk factors such as age, sex, race, family history, and concurrent conditions such as diabetes or high cholesterol levels. Any borderline patient with two or more factors plus certain levels of hypertension would warrant treatment. Mild hypertension alone, however, might be treated at first with a low-sodium diet, weight loss, and exercise. If drug therapy was indicated, Freis recommended starting with a thiazide diuretic, then adding other drugs as needed, in a stepped-care regimen. A related question was about patient compliance with treatment: hypertension medications often have unpleasant side effects, and patients complain that they feel worse with them than without. Always sensitive to the patients' treatment experience, Freis stressed the need for monitoring and adjustment of drug treatment, emphasizing the variable reactions to different drugs. He cautioned against a "one-size-fits-all" approach to hypertension treatment. He also advocated making patients partners in their own care by having them use home blood-pressure gauges to monitor their progress.
Another challenge in hypertension treatment emerged in the 1980s, when thiazide diuretics, a mainstay of antihypertensive therapy, provoked concerns. Some reports indicated that the diuretics, by depleting potassium levels, could pose a danger to certain patients, inducing cardiac arrhythmia and even heart attacks. Other reports linked diuretic use to higher cholesterol levels. At the same time, with the advent of newer hypertension drugs such as angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers (which relax the blood vessels by keeping calcium from entering the muscle cells in the vessel walls), some physicians questioned the need for "obsolete" drugs such as diuretics. Freis, who had pioneered the use of the thiazides and used them effectively and safely for thousands of patients, energetically defended their use. He and his colleagues did several surveys of the medical research literature, searching for definitive evidence that diuretics were dangerous. They found none. To his disappointment, use of diuretics for hypertension treatment declined nonetheless. His argument was vindicated by the ALLHAT (Antihypertensive and Lipid Lowering Treatment to prevent Heart Attack Trial) study (1994-2002), which showed that treatment with diuretics controlled blood pressure better, and was significantly better for preventing cardiovascular disease events when compared to treatment with ACE inhibitors, calcium channel blockers, or alpha-adrenergic blockers.
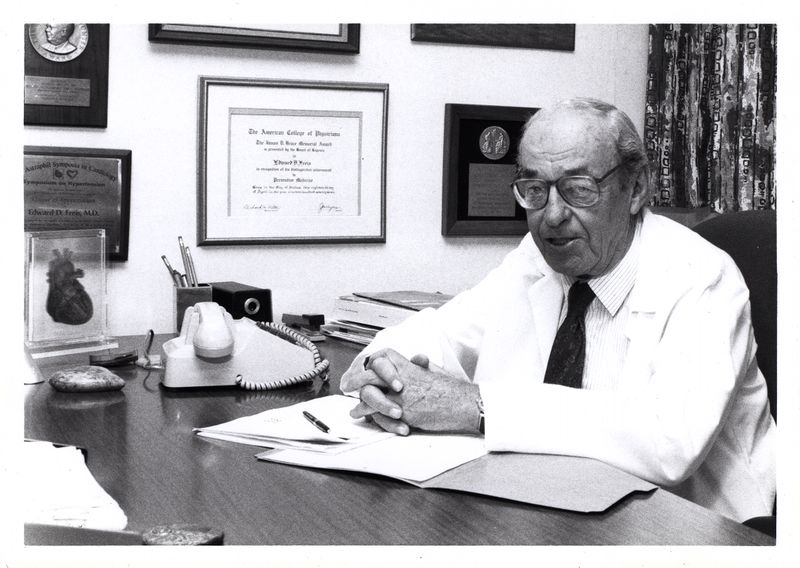
By the time Freis retired in 1987, he had been investigating the treatment and mechanisms of high blood pressure for over forty years, and had trained several generations of cardiologists. He was named Distinguished Physician by the VA Medical Center and Professor Emeritus by Georgetown University School of Medicine, and continued to serve as an advisor to ongoing clinical studies, and to publish about hypertension for nearly two decades. Georgetown University awarded him an honorary doctorate of science in 1995, and in 2000 he was given the first Stevo Julius Award for Education in Hypertension by the International Society for Hypertension, in recognition of his years of leadership in that area of cardiovascular medicine. Despite declining health, Freis stayed as active as possible. On his ninetieth birthday, he celebrated with friends, colleagues, and family, played Chopin on the piano, and recited Hamlet's soliloquy from memory. At the time of his death on February 1, 2005, Freis was just finishing a second hypertension book for a popular audience.
According to the National High Blood Pressure Education Program, one of every three Americans currently has high blood pressure, i.e., pressures greater than 140/90 mm Hg. Freis, in his last years, was disappointed that the incidence of hypertension was still so high, and that only about one-third of those with hypertension receive treatment adequate to keep their pressure at normal levels. Clearly, there is still much work to do on this problem. Yet, in 1972 less than 25 percent of Americans knew the relationship between hypertension and cardiovascular diseases; only half of those with hypertension were aware of their condition, and less than one-third were receiving any kind of treatment. Those numbers have increased greatly since then. And, although coronary heart disease (CHD) and stroke--two of the major complications of untreated hypertension--are still the first and third causes of death, respectively, in the United States, the mortality rates from those diseases have dropped dramatically. Between 1972 and 1994, the mortality rate from CHD per 100,000 declined from 195.4 to 92.4. The mortality rate from stroke per 100,000 declined from 64.6 to 26.7 during the same period. Such changes have stemmed in great part from Freis's many decades of work. He repeatedly demonstrated that hypertension, however "normal" or "benign" it might seem, had serious consequences, and that treatment could prevent those consequences.